Researchers from Stanford University have developed a way to replicate a patient’s blood vessels in a 3D-printed model, a cheaper, yet as effective, method as commercially available models for training medical students in interventional radiology vascular access.
The study was presented at the Society of Interventional Radiology’s 2018 Annual Scientific Meeting.
Interventional Radiology
Compared to open surgery, interventional radiology is a less-invasive method to diagnose and treat diseases in organ systems.
Interventional radiologists insert a catheter through a major artery under ultrasound guidance to reach internal organs or blood vessels. Due to its lower risk, pain, recovery time and, in most cases, cost, interventional radiology is largely preferred by patients.
However, the current model used to train medical students is both too expensive and unable to replicate each patient’s unique anatomy.
For interventional radiology, the market price for commercially available simulation devices is between $2,000 and $3,000 each, with an additional $500 for replacement inserts for punctured portions.
Plus, because the current models follow a general version of human anatomy, students often feel unprepared going into an actual treatment.
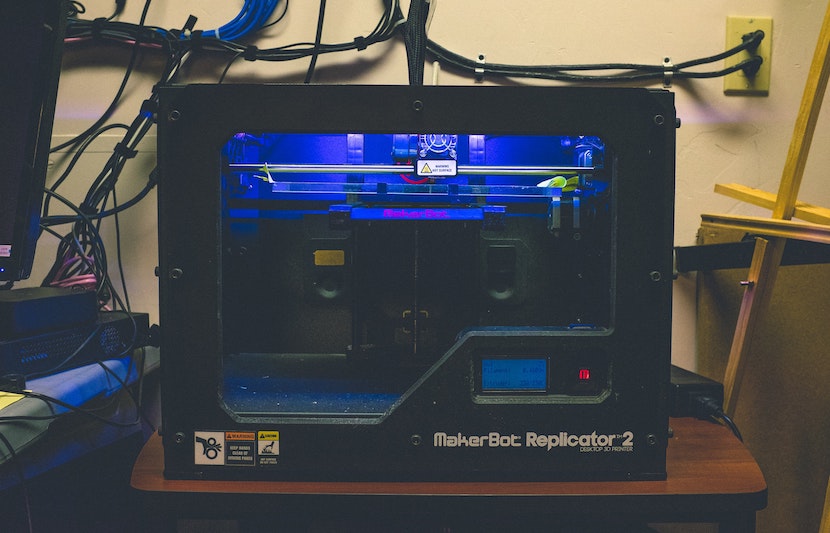
But now researchers at Stanford University are using a 3D printing method to solve this problem.
“The 3D-printed models that we developed can be produced inexpensively and more realistically to simulate a patient’s individual anatomy, especially for those institutions that already have 3D printing available,” said Alexander Sheu, an interventional and diagnostic radiology resident at Stanford University School of Medicine and lead author of the study.
The study
Unlike a generalized version of the current model, the researchers’ 3D-printing technology can reproduce a patient’s exact vessels based on a CT scan and produce an ultrasound-compatible vascular access model that is unique to that patient’s anatomy.
To best adapt the 3D-printing technology to a student’s simulation session, the researchers used a tissue-mimicking material that was durable enough to withstand punctures, but still felt realistic. This tailoring allows students to practice with variations in anatomy before they encounter them during an actual treatment.
The researchers hope this will help to lower complication rates.
Then, the researchers gathered 32 medical students to test how effective their 3D model is in preparing the students, as compared to commercially available models.
Randomized into two groups, the students completed a simulation experience developed by the researchers, simulating ultrasound-guided access through the femoral artery in the groin.
The results
The researchers found that their 3D-printed model is just as effective at training medical students in interventional radiology procedures.
Before the simulation exercise, 73 percent of the 3D group and 76 percent of the commercial-model group indicated that they did not feel confident in performing the procedure.
After the exercise, the majority of students in both groups agreed that their respective models were easy to use (93.3 percent in 3D model and 94.1 percent in commercial model) and helpful for practice (93.3 percent in 3D model and 94.1 percent in commercial model).
Additionally, students in both groups showed a similar amount of increase in confidence in performing the procedure.
The researchers are excited that their model will provide not only affordable, but also realistic training opportunities to more trainees.
“This model is customized to a patient’s unique anatomy, providing students a more realistic experience and ultimately allowing for better preparation before they perform procedures on real patients,” said Sheu.
The next step
The researchers aim to continue researching to better understand the benefits that their model can provide to trainees.
“We would like to extend use of the model to resident physicians, fellows, and faculty,” said Sheu.
“Evaluation of the model with validated objective measures of competency would be valuable for additional assessment of efficacy.”
The team is also looking to develop 3D-printed models for other parts of the body, so their model can be used for jugular vessels and vessels in the abdomen, and not just for the femoral vessels, according to Sheu.