Led by Dr. Sterghios Moschos, associate professor in cellular and molecular sciences at Northumbria University at Newcastle in England, a team of researchers has created a “new, faster and safer way” for mass screening for the Ebola virus.
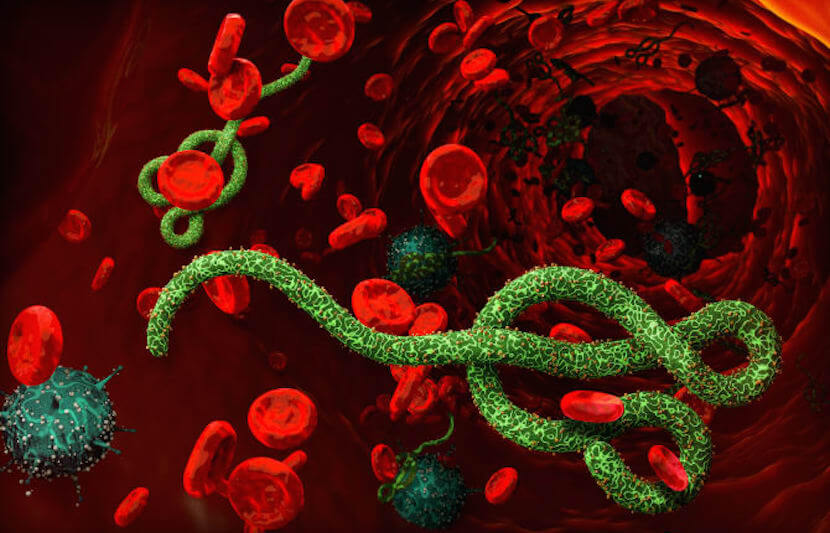
First identified in 1976 in two contemporaneous outbreaks in South Sudan and the Democratic Republic of Congo, the Ebola virus is fatal if not treated promptly and properly. Risk of death is high, between 25 to 90 percent in past cases, according to figures released by the World Health Organization. The deadliest outbreak was the 2014-2016 West African outbreak, which struck more people and caused more deaths than all previous outbreaks combined.
The researchers believe that their new diagnostic platform, known as EbolaCheck, will make the screening process both faster and safer, helping to curb the spread of the disease.
During the 2014-2016 outbreak, the screening process took between 5-8 hours and required patients to provide a blood sample in a specialized lab staffed with highly trained specialists. Such facilities are rare to begin with, and are not easily accessible by patients, particularly in economically disadvantaged countries.
In contrast, EbolaCheck requires only a drop of blood, which can be accomplished by “pin pricking” a patient’s finger, and can be completed in less than 70 minutes. The process can be done anywhere where there has been a recent outbreak, requires little training to carry out, and cuts the cost of diagnosis.
According to the researchers, this new technology has proven comparable to the kind of testing that is carried out in medical laboratories, offering patients a system that will ensure a safe and reliable diagnosis.
This new technology is not limited to screening for the Ebola virus. It could be used to screen for other viruses, including Zika, MERS, SARS, flu, and dengue viruses, as well as bacterial and parasite infections, including meningitis and malaria. This could be done because the technology “detects and measures genes and genomes.”
“The development of this pioneering technology could essentially save lives and reduce the spread of the disease, which is crucial in a humanitarian crisis,” said Moschos in a statement. “Due to there being no further cases since it was developed, to date, it has not been possible to take the test out of the lab, into the field, where the patient needs it. However, it can be deployed anywhere – the frontline in Africa where this disease is found, as well as international airports and ports – to help stop the disease from spreading and to prevent disruption of international trade and travel. It could also be used in the diagnosis of other infectious diseases, as well as bringing genetic testing to the shop front, for example in a pharmacy or a GP surgery.”
The 2014-2016 deadly outbreak should serve as a lesson in responding to future outbreaks, according to Moschos.
“There have been substantial lessons from the outbreak,” he said. “For example, how not to assume anything when it comes to hemorrhagic fevers regarding their cause — it could be something as common to the local environment as malaria was to West Africa, or it could be something as unexpected as Ebola virus was. How to anticipate and deal with conspiracy theories that get in the way of actual care for the individuals afflicted and the communities affected. How to deploy measured and appropriate responses, and not resort to knee jerking. In line with this principle, deploying a technology that serves a single purpose, e.g., screening for the Ebola virus, is not appropriate, unless screening for that virus is of utmost immediate urgency.”
It is crucial also, Moschos explained, that the best of medical research should be made commercially viable in order to tackle upcoming challenges in health care.
“Screening for so-called neglected tropical diseases, treating these diseases found in low income countries, and treating rare genetic diseases found usually in the west are two sides of the same coin: how to make the best of research science a commercially logical proposition that motivates the production of these forms of health care without relying on charitable support, fear for developed nation safety, or extortionate pricing,” he said. “We are on the cusp of a fundamental change in the economy of health care, and the lessons from the Ebola outbreak can and will change how we do things in modern medicine.”
The research uses proprietary technology, known as “QuRapID,” developed by BioGene Ltd, and is funded by a grant from Elrha’s Research for Health in Humanitarian Crises (R2HC) Programme.
The research involved several organizations, including BG Research Ltd, the University of Westminster, Public Health England, Flurogenics Ltd, Diagnostic Systems Division and Virology Division of the U.S. Army Medical Research Institute of Infectious Diseases, and Kwame Nkrumah University of Science and Technology in Ghana.