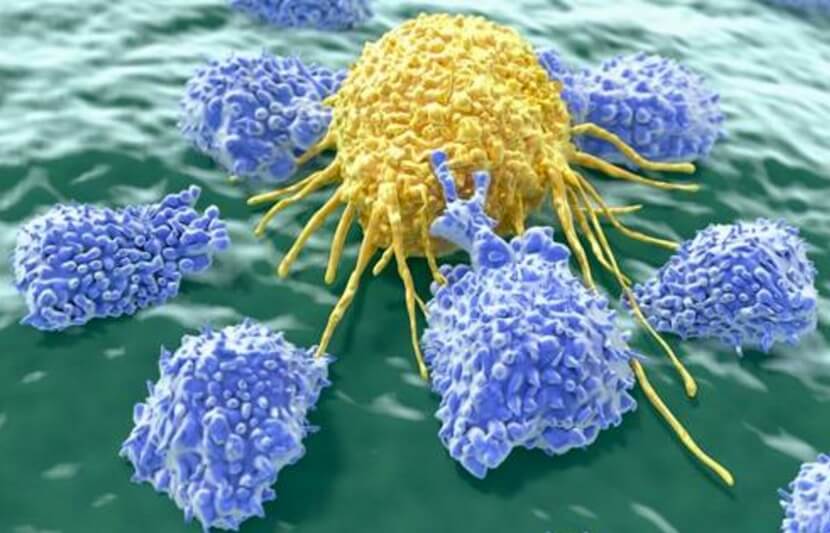
Researchers at Cardiff University in the UK have developed two unique ways of attacking cancer cells. The first method targets cancer-ridden T-cells without harming healthy ones, while the second method uses genetically engineered healthy T-cells to destroy cancerous cells.
T-cells, a type of white blood cell, are a part of the immune system that help us fight bacterial and viral infections. These cells can be broadly divided in two types: killer T-cells and helper T-cells. As the name implies, killer T-cells can kill certain cells, including foreign cells, cancer cells and cells infected with germs. Helper T-cells play a major role in controlling and regulating the body’s immune system by helping other white blood cells eliminate the foreign, cancerous or infected cells.
Attacking Cancerous T-Cells Without Harming Their Healthy Counterparts
Lymphoma is a type of cancer that begins in white blood cells called lymphocytes. In patients with lymphoma, the lymphocytes begin to multiply uncontrollably. Since it is a blood cancer, operating is not possible.
Traditional lymphoma treatment methods, such as radiation and chemotherapy, are universally destructive, killing healthy and cancerous cells indiscriminately. Unfortunately for patients, inoperable cancers are currently only treatable with these damaging and dangerous techniques. Developing a method of cancer treatment aside from surgery that can differentiate between healthy and cancerous cells is essentially the holy grail of oncology.
In the case of lymphomas specifically, there are two varieties — B-cell and T-cell lymphoma. B-cell lymphoma is now, thanks to advances in immunotherapy, treatable. (Immunotherapy is a form of treatment that uses the body’s own immune cells to fight cancer.) T-cell lymphoma, however, which is rarer and deadlier, is in desperate need of a new form of treatment.
The problem with treating T-cell lymphoma is that traditional treatment methods lower the general count of T-cells in the body, rather than specifically targeting cancerous ones. T-cells are vital to the immune system, so the brute-force destruction of all T-cells via chemotherapy would put patients in serious danger.
The research team at Cardiff University, however, has found a way to target only cancer-ridden T-cells while leaving healthy T-cells unharmed.
T-cells are formed using one of two duplicated copies of the T-cell receptor gene, known as C1 and C2, decided by a random process. Given this random nature, approximately half the T-cells in our bodies are genetically C1 and the other half are C2.
In T-cell lymphoma, the cancer starts from a single T-cell and only spreads to T-cells of the same gene. If the origin cell is C1, then only C1 T-cells will be cancerous while C2 T-cells would remain healthy, or vice versa.
The team’s method makes it possible to eliminate T-cells based on whether they use the C1 or C2 gene. The team has demonstrated that targeting of C1 T-cells can kill C1 cancers without harming any normal C2 T-cells, so these cells can continue to protect the body.
“We wouldn’t last a week without the essential job our T-cells perform by protecting us from infection,” Professor Andrew Sewell from Cardiff University’s School of Medicine said in a statement. “The devastating effects of low numbers of just one type of T-cell are all too evident in HIV/AIDS.”
The research team is currently working with Autolus, Ltd., a biopharmaceutical company based in London, to begin clinical trials.
“The chimeric antigen receptor (CAR) targeting TRBC1 positive T-cell lymphomas forms the basis of AUTO-4, a CAR T-cell product currently being developed by Autolus,” said Dr. Mateusz Legut, who co-authored the study while undertaking a Cancer Research UK funded PhD in Sewell’s laboratory. “The phase I clinical trial testing AUTO-4 should commence in 2018.
“At the same time, another CAR product targeting TRBC2 positive T-cell lymphomas is being developed. We expect that the remarkable clinical success which has been observed with CAR therapies targeting B-cell malignancies can now be replicated in T-cell malignancies, by specific targeting of either TRBC1+ or TRBC2+ lymphomas.”
Sewell expects that Adaptimmune, a company that is “already applying TCR gene transfer in the clinic” and other companies “will pick this approach up for treating patients,” he said.
The paper is published in Nature Medicine.
Using CRISPR Genome Editing to Attack Cancer Cells
Legut and Sewell were also involved in the study on genetically engineering healthy T-cells to destroy cancer cells.
This team removed the non-cancer specific receptors of T-cells via genome editing, allowing these modified cells to kill only cells corrupted by the cancer.
The team’s modified cells are stronger than ones prepared under current methodology, explains Legut, who led this study.
“Up until now, T-cells engineered to fight cancer had two kinds of receptors – the therapeutic one that was added in the lab, and their own naturally existing one,” he said in a statement. “Since there is only limited ‘space’ on a cell for receptors, cancer-specific ones need to compete with the cell’s own receptors to perform their function. More often than not, the cell’s own receptors win that competition, and leave ‘space’ for only a very limited number of newly introduced, cancer-specific receptors, which means that T-cells engineered with the current technology never reach their full potential as cancer killers.”
Basically, the researchers remove the receptors in T-cells that target general pathogens and replace them with receptors that specifically target cancer.
“The improvement in the sensitivity of cancer recognition that can be achieved by editing out the existing natural receptor and then replacing it with one that sees cancer cells is remarkable,” Sewell said in a statement.
Editing T-cells so that they can focus entirely on cancerous cells increases the efficiency of immunotherapy by, in essence, enlisting a cellular task force with the sole purpose of destroying cancerous cells.
“I believe that our improved method of making cancer-specific T-cells will guide a new generation of clinical trials and be used by researchers in the laboratory to discover new cancer-specific T-cell receptors and new targets for cancer therapy,” Professor Oliver Ottmann, head of hematology at Cardiff University, co-lead of the Cardiff Experimental Cancer Medicine Centre (ECMC), and co-author of the study, said in a statement.
The study was performed in a laboratory and has not yet proceeded to clinical trials.
The paper is published in Blood.
This research team also includes Dr. Garry Dolton and Afsar Ali Mian.